Manning Fund is …
Recent News
21 E-Commerce Startup Ideas for New Entrepreneurs
Want to start your own e-commerce business in Canada and sell goods to the buying-hungry Canadian market but need help figuring out your e-commerce startup ideas?
We understand that it’s a huge leap. Launching something as massive as your own e-commerce business is daunting, especially when you don’t have the right ideas.
Well, stick around and read on because we’ve got 21 of them for you. We’ve researched and scoured all corners of the internet.
And we came up with a comprehensive list of 21 of the freshest profitable …
Top 5 Latest Technological Innovations
Technology is a fast-paced industry that never seems to be satisfied with just one new tech innovation. It is always looking for the next big thing, and sometimes it can seem like there are too many innovations to keep track of.
Every day, scientists and engineers worldwide create new technologies that can help us live more efficiently or explore our universe more thoroughly.
Five Technological Innovations
5G Network
5G, as the latest technological innovation, is the upcoming fifth…
The Advantages and Disadvantages of Opening a Vaping Business
Vaping has become famous all over the globe because of the Vaping suppliers. Smokers are beginning to realize the benefit of switching to a healthier alternative, and being able to choose thousands of different flavors to vape also excites them. For that reason, they begin to choose it over smoking.
If you are considering opening up a business, then study the pros and cons.
The Pros of Setting Up a Vaping Business
The business offers you different opportunities.
Aside from being a substitute for smokers, cannabis users also prefer vaping CBD. As a…
The Top Tech Entrepreneurs in Canada That You Need to Watch in 2021
Now that the world is getting ready for a fresh restart, people are looking for inspiration for their goals this 2021. Below is a rundown of some of the biggest tech entrepreneurs in Canada which you surely need to watch this year.
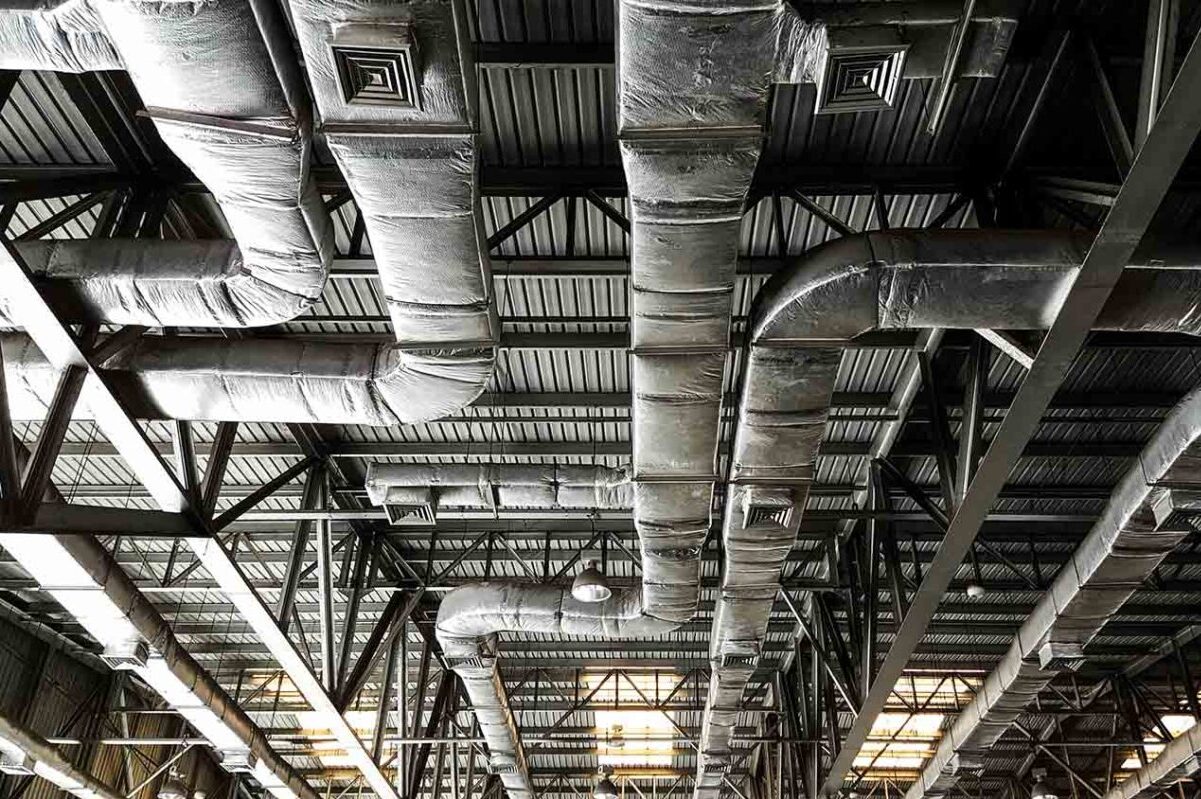
1. Sam Ramadori
Sam Ramadori and his team of innovators at BrainBox AI have been well-renowned for building cutting-edge buildings through HVAC systems. HVAC systems have been figured by many scientists to diminish the escalation of airborne diseases. Thus, it is predicted that the world will use the service of companies like Sam Ramadori’s BrainBox AI.
2. Sage Franch
…
These Canadian Start-Up Tech Companies Are Hiring This January 2021
These startup companies have so much to offer to job-seeking individuals; highly competitive salary and benefits, state-of-the-art work facilities, work-life balance, as well as the opportunity to take part in valuable and high-impact projects.
1. eSight
eSight is a Toronto-based company that develops electronic glasses and offers innovative tools to help blind people see.
When you work at this company you get the opportunity of changing blind people’s lives for the better. You also get generous vacation leaves, as well as extensive healthcare and dental coverage.
The company is currently hiring for the …
The Top 3 Biggest Tech Success Stories of 2020
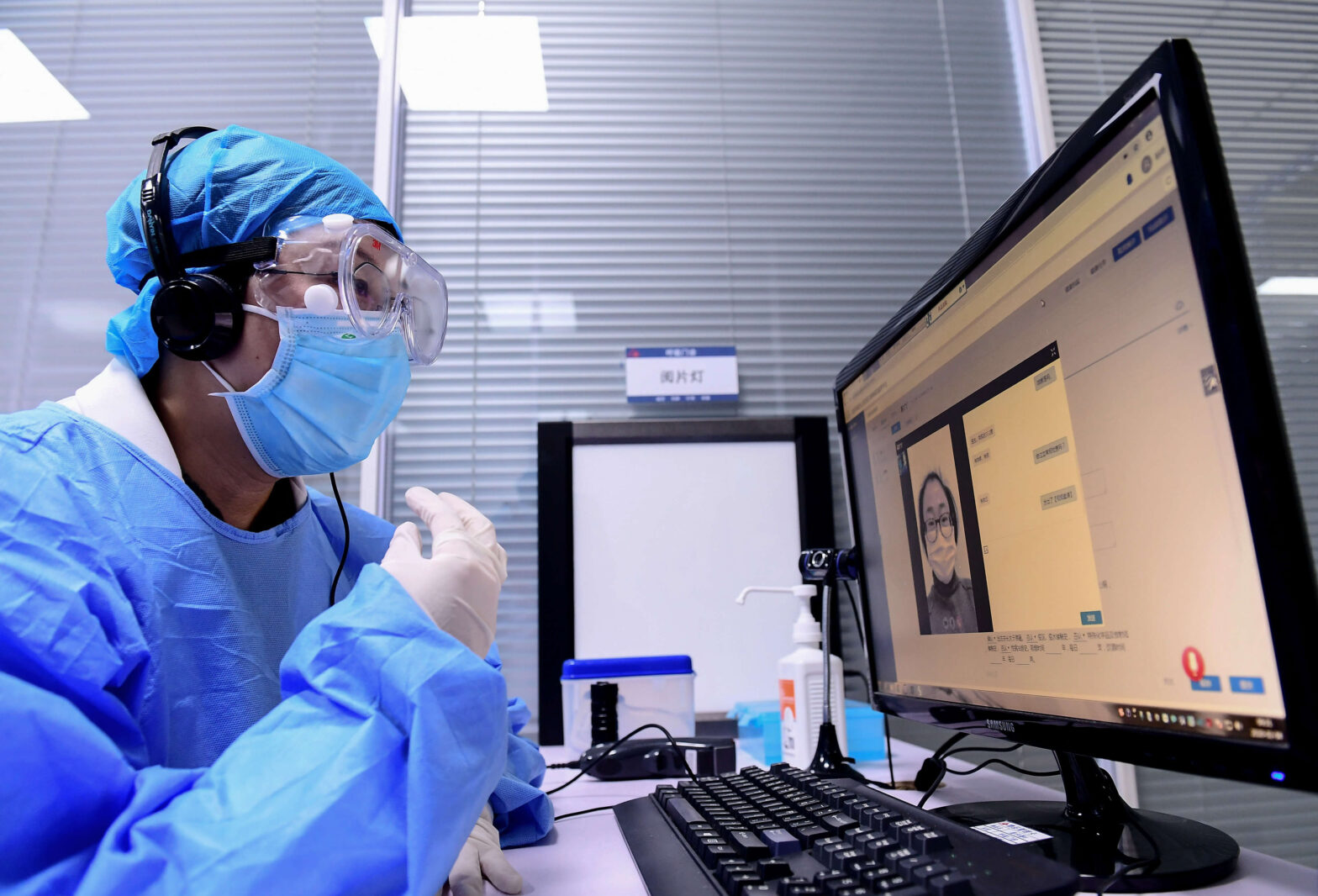
Although Covid-19 has undeniably made a big chunk of the headlines in 2020, the past year has also been a year of many tech success stories that brought hope, solidarity, and scientific progress.
Below is a list of some of the biggest tech news in the past year.
1. The Development of Vaccines to End Covid-19
The development of covid-19 vaccines has brought unprecedented collusion between private and private institutions across the globe. These vaccines have been created in a record time of about 10 months only when vaccines typically take years to be developed. Nevertheless, the vaccines are finally here and it is …